 FAMILY HANDOUTS
FAMILY HANDOUTSEarlier this year, a new drug to treat severe alopecia – an autoimmune condition that causes hair loss – was given the green light for NHS use. Some want to try it, others don’t – and some think it can be life-changing.
Alicia Pylypczuk is a grumpy A&E doctor who took her own life after years of struggling with depression triggered by alopecia.
It’s been four years since her death and Alicia’s stepfather, Alan Green, is convinced she’ll take a new drug.
The 29-year-old from Manchester began suffering episodes of hair loss at a young age, while studying for her A-levels.
He was told by a dermatologist that there was nothing he could do to stop the alopecia, according to Alan, who believed the psychological effects caused him to lose his identity.
 Family handouts
Family handouts“He was a thoughtful, knowledgeable and dedicated doctor,” Alan said.
He enjoys spending time with his friends and his musical talent, he added, but the situation affects the way he thinks people see him.
“Everyone told her that without the wig she was a very beautiful woman, but she didn’t see it. She only saw it as ugly and unattractive – everything began to affect the rest of her life.
In February this year, a A new drug, ritlecitinib, is recommended on the NHS in England and Wales for the first time for patients aged 12 and over with severe alopecia.
A month later in April approved for NHS use in Scotland and in Northern Ireland.
Alopecia is caused by the immune system mistakenly attacking the hair follicles at the root of the hair, causing it to fall out.
These drugs reduce the activity of the part of the immune system that is involved in the inflammatory reaction.
Evidence from clinical trials shows that nearly 25% of adults and adolescents taking the treatment, under the brand name Litfulo, experienced significant hair regrowth covering 80% or more of the scalp within 24 weeks.
If treatment had been available before Alicia died, she would have had the opportunity “with both hands”, Alan said.
“It is very difficult to live in the mind of someone with alopecia.
“I don’t think people understand the problems that people with alopecia go through – and more people need to talk about it.”

Alopecia and Me
A new drug aimed at encouraging hair growth for people with alopecia has been approved for use on the NHS in the UK – but is the treatment worth it for everyone?
If you’re in the UK, watch it on BBC iPlayer

Newcastle actor Sam McGregor recently moved to London with ambitions to launch his acting and writing career.
But soon after moving to the capital, he quickly lost his eyelashes and eyebrows. Clumps of hair began to fall out.
“I’m not shy,” Sam explained. “But when you notice how pale my scalp is, you go ‘woah’. There was a period of two weeks initially when I was uncomfortable.
“When people associate you with no hair, they think it’s more than it is.”
 Caden Elliott
Caden ElliottHe said bald men should act in “certain parts” on TV, and he asked: “What’s my casting bracket now?”
But then he realized that he “stands out more”, and in the end it became a unique selling point.
“It’s an advantage,” he said. “But I’m still not sure how it’s all going to work out.”
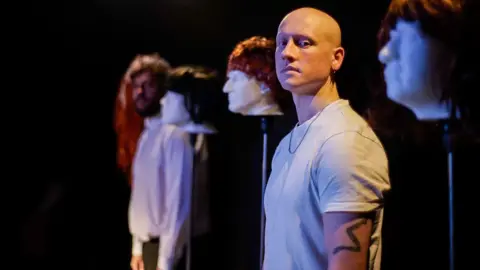
Inspired to inform people about what alopecia is like, Sam created and presented a play about the condition at the Edinburgh Fringe Festival last August.
The show Really, Madly, Baldy tackles problems faced by both men and women – including those that come with sudden hair loss.
“I’ve had a mix of bad times and frustrating times,” Sam explained.
He heard offensive things, “but because I was not comfortable with my hair loss, I took it on board and thought: I can write this and do something later”.
Sam said he doesn’t like “singing (himself) praise” about what alopecia has done for him and feels like he’s in the minority.
“On the whole, I can work. My hair is falling out and all the work is starting to flood. The play is about what I can give, what I can do to let others know about it.
Sam says he knows people who have taken ritlecitinib and who have seen hair regrowth.
“It’s great that it’s out there and people can try it,” Sam said. “But I personally wouldn’t take it.
“I wouldn’t say no, but I like my alopecia now.”

Glasgow student Megan McGready has also learned to cope with her situation and is now supporting other young people going through the same thing.
“Going into high school, my hair was falling out and it was scary,” Megan recalls. I have several days off. It was terrible and I got bullied a lot.
“I’m afraid to touch my hair and I’ll keep going out in the bathroom, seeing if I can fix it or see if it looks.”
Without telling anyone, when she was 13 years old, Megan took scissors and cut and shaved the hair she had and for her it was a way to control her condition.
“I feel freer,” he said. “I feel more responsible.”
However, alopecia made him change his long-term life plans.
Megan wanted to go to sports coaching, but faced the difficulty of balancing sports with wearing wigs, which can lead to overheating, as well as painted-on eyebrows.
 Unknown
UnknownMegan is always keen to research alopecia treatments, so she was delighted to see ritlecitinib accepted in April by the Scottish Medicines Consortium.
They are ready to try new treatments.
“This new medicine can make my life easier,” he continued.
“I wake up in the morning and I don’t have to worry about my eyebrows, I can just go out and have fun or worry about the heat wearing a wig.
“If I could get my hair back, I would appreciate it more. This new drug is sure to change the lives of many people.
Although ritlecitinib has been approved for use by the NHS, few patients have been prescribed it.
A month’s worth of pills cost the health service just under £1,000, and regular blood work is required to monitor progress.
But Alicia’s stepfather sees this as a big step in the right direction.
“It’s a prospect,” Alan said. “We don’t know how effective it will be — will it be effective for everyone?” Alan asked.
“Time will tell. This is an opportunity for the alopecia community to have hope.
If you have been affected by the issues in this story, help and support is available through BBC Action Line





